Opinion: HealthTrust's decision to drop anti-obesity medications is a step back in the fight against a chronic disease

Amanda Andrade-Rhoades / AP Amanda Andrade-Rhoades / AP
| Published: 04-09-2025 4:43 PM |
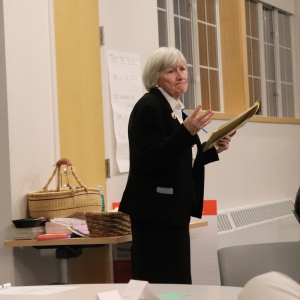
Joseph Zucchi is a physician assistant and clinical supervisor at Transition Medical Weight Loss in Salem.
Recently, I received a letter from CVS Caremark informing me that effective March 1, HealthTrust would no longer cover anti-obesity medications for my patients who have the HealthTrust Prescription Benefits Plan.
As a physician assistant specializing in obesity medicine and the clinical supervisor at Transition Medical Weight Loss in Salem, this news was deeply troubling.
HealthTrust, an organization providing health benefits to many of New Hampshire’s public sector employees, including thousands of teachers, school staff and municipal workers, has decided to discontinue coverage of this entire class of medications. The immediate impact will be felt by dozens of my patients who have made incredible strides in their health and quality of life with the help of these medications.
I’ve witnessed firsthand how anti-obesity medications (AOMs) can transform lives. These are not a quick fix; they are vital tools in managing obesity, a chronic, relapsing disease. HealthTrust’s decision to eliminate this coverage doesn’t just represent a simple policy change. It directly undermines the health and well-being of dedicated teachers, public sector employees and their families who depend on these medications to lead healthier, more productive lives.
Consider some real-life examples of my patients: A teacher who, under my care, lost 100 pounds, was able to maintain this weight loss and successfully discontinued two blood pressure medications. Or the municipal worker who shed 60 pounds and saw his sleep apnea go into remission, finally enjoying restful sleep for the first time in years. These stories showcase the impact of sustained medical weight management.
Obesity is often misunderstood and stigmatized as a lifestyle choice or a failure of willpower. However, years of clinical research and experience clearly show that obesity is a complex medical condition influenced by genetics, hormonal balance, psychological factors and environmental conditions. Just as hypertension and diabetes require long-term medication management, obesity often requires ongoing medical support to properly manage and maintain significant weight loss and health improvement.
Recent studies demonstrate this clearly. For example, in the SURMOUNT-4 trial involving tirzepatide (Zepbound), participants achieved an average weight loss of 20.9% after 36 weeks on the medication. However, those who were switched to placebo at that point experienced significant weight regain, going from 20.9% down to 9.5% total weight loss at week 88. They regained more than half of their previously lost weight.
Article continues after...
Yesterday's Most Read Articles
 Concord superintendent joins over 100 school leaders in signing controversial DEI certification, but says equity work will continue
Concord superintendent joins over 100 school leaders in signing controversial DEI certification, but says equity work will continue
 Another lawsuit delays Steeplegate Mall demolition
Another lawsuit delays Steeplegate Mall demolition
 Propane tanker truck rolls over on I-93, holds up traffic
Propane tanker truck rolls over on I-93, holds up traffic
 Federal judge finds Bow School District’s actions ‘entirely reasonable’ in transgender athlete protest by parents
Federal judge finds Bow School District’s actions ‘entirely reasonable’ in transgender athlete protest by parents
 Transitional housing at risk after New Hampshire lawmakers vote to sell state-owned building
Transitional housing at risk after New Hampshire lawmakers vote to sell state-owned building
 New Hampshire set to ‘welcome home’ veterans with new 15-acre campus in Franklin
New Hampshire set to ‘welcome home’ veterans with new 15-acre campus in Franklin
For patients, this isn’t simply about a number on the scale. Weight regain means renewed battles with conditions like diabetes, sleep apnea, hypertension, joint pain and heart disease. Meanwhile, those who continued the medication not only sustained their weight loss but achieved an average of 25.8% total weight loss by week 88.
In practice, we see the strong impact these medications have on patients every day. Patients who struggled for decades to lose weight through diet and exercise alone find themselves empowered and successful with the help of one of these medications. Their quality of life improves dramatically, as does their productivity, mental health and overall healthcare utilization. Removing medication coverage not only reverses these positive gains, but it places additional financial and emotional burdens on individuals already managing a challenging medical condition.
Understandably, HealthTrust and other insurers face increasing pressure to control healthcare costs, especially as spending on obesity treatments increases. However, short-term financial savings achieved by cutting these medications pale in comparison to the long-term healthcare costs associated with untreated obesity such as expenses from diabetes complications, heart disease, joint replacements and disability.
The sad truth is that patients who lose access to effective anti-obesity medications often turn to risky, compounded or unregulated alternatives, or they simply suffer in silence as their health deteriorates. This is an unacceptable outcome for anyone invested in the long-term health of our state’s workforce.
HealthTrust’s decision may be motivated by cost savings but the health and financial repercussions down the road will likely prove far more costly. As a healthcare provider, I have a duty to advocate for responsible healthcare policies driven by an understanding of obesity as the chronic medical condition that it is.
I urge HealthTrust and other insurers in New Hampshire to reconsider their policies. Let’s invest in evidence-based obesity treatments that yield true, long-term savings, both financially and in the lives and well-being of Granite Staters. Obesity is not a choice, but supporting effective treatment certainly is.




 Opinion: An attack on the legal profession is an attack on us all
Opinion: An attack on the legal profession is an attack on us all
