Area nursing homes warn new federal staffing standards could reduce capacity

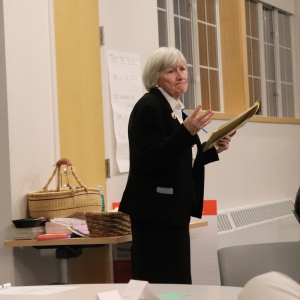
Maplewood Nursing Home in Westmoreland. Hannah Schroeder—Keene Sentinel staff photo
| Published: 05-20-2024 10:00 AM |
New staffing mandates from the federal government will likely reduce the number of nursing home beds available in the Monadnock Region, officials say, leaving people who need a higher level of care less able to access it.
The new rules, which were finalized by the Centers for Medicare & Medicaid Services on May 10 after an executive order by President Joe Biden, set minimum staff-to-patient ratios — which previously weren’t spelled out at the federal level — and require a registered nurse to be on site at all times.
The mandates will be implemented over the next two to three years, although some rural facilities will have up to five years to meet the requirements. Even with that exception, local nursing home administrators say they are worried.
“The impact of the rules could be that we close more beds,” said Kathryn Kindopp, administrator of Maplewood Nursing Home in Westmoreland, which is run by Cheshire County.
National analysis from the American Health Care Association shows that to meet the mandates, long-term care facilities nationally would need to hire about 100,000 additional staff. Finding those workers is a challenge all over the country, but in New Hampshire — where nursing home officials say health care staff simply aren’t available due to high demand, low supply of new graduates and pandemic-related retirements — it could prove impossible.
Facilities will likely need to reduce the number of beds in service to meet the required ratios, administrators say.
The mandates lay out specific hours of care per day that each nursing home resident must receive. Essentially, that translates to a specific staff-to-resident ratio. Hillsborough County Nursing Home in Goffstown is currently meeting the levels outlined by the new requirements, but just barely.
“On any given day, if we had a nurse call out we wouldn’t be meeting that threshold,” said administrator David Ross. It’s a similar situation at Maplewood, Kindopp said, with the Cheshire County facility currently meeting some of the new requirements, but not others, depending on how certain staff are counted.
Article continues after...
Yesterday's Most Read Articles
 Concord superintendent joins over 100 school leaders in signing controversial DEI certification, but says equity work will continue
Concord superintendent joins over 100 school leaders in signing controversial DEI certification, but says equity work will continue
 Another lawsuit delays Steeplegate Mall demolition
Another lawsuit delays Steeplegate Mall demolition
 Propane tanker truck rolls over on I-93, holds up traffic
Propane tanker truck rolls over on I-93, holds up traffic
 Federal judge finds Bow School District’s actions ‘entirely reasonable’ in transgender athlete protest by parents
Federal judge finds Bow School District’s actions ‘entirely reasonable’ in transgender athlete protest by parents
 Transitional housing at risk after New Hampshire lawmakers vote to sell state-owned building
Transitional housing at risk after New Hampshire lawmakers vote to sell state-owned building
 New Hampshire set to ‘welcome home’ veterans with new 15-acre campus in Franklin
New Hampshire set to ‘welcome home’ veterans with new 15-acre campus in Franklin
Once the federal mandates are law, the nursing home will need to build in a buffer to account for sick days and staff absences, which could mean a reduction in beds if the home can’t hire more personnel, Ross said of the Hillsborough County home.
At that facility, 50 of 300 beds are out of service because of staffing shortages — meaning the facility is not accepting patients for those beds. At Maplewood, 40 out of 150 beds are already out of service. The problem isn’t unique to county-run homes: Nationally, four out of five nursing homes don’t currently meet the requirements laid out in the new order, according to Kaiser Health News.
While the rules were implemented with the goal of improving care, according to the President, they don’t come with increased pay rate from Medicare or Medicaid, prompting the The American Health Care Association to call them an “unfunded mandate,” Kaiser Health News reported.
Between the two local nursing homes, 20 percent of licensed beds can’t be used, although when to close beds is up to the discretion of the nursing home administrator, since current mandates only require “sufficient” staff.
That contributes to long waits for people who need nursing-home level care: Maplewood has 81 people on its waiting list, and in Hillsborough County, the list is more than 100 people long. Some people remain in their homes with inadequate care, while others wait in hospitals until a long-term bed becomes available, Ross noted.
“Reducing the number of people that we’re able to serve, that would be catastrophic,” he said.
Both Kindopp and Ross say that they are intentional about maintaining a staff-to-patient ratio that is safe and effective, even when that means closing beds.
“We made the conscious decision to reduce our occupancy to maintain a level of care that we’re comfortable with,” Ross said.
The federal mandates are a one-size-fits-all approach that remove the discretion from the facility, he added.
The rules are meant to promote a higher level of care in nursing homes. Research shows that more staffing can improve outcomes for nursing home patients, but Kindopp said doing so is not just about increasing staff numbers.
“It’s been my experience over the years that high quality care … does not come from numbers alone,” she said. “It’s really about individuals who have the calling to care for our vulnerable elders.”
The rules could increase the reliance on contract workers, which are more expensive than employees. Between 2022 and 2023, Hillsborough County Nursing Home increased its spending on travel nurses and staff by 10 times, Ross said previously.
In addition to driving up costs, contract workers, who often work at a facility for a short period of time, can be distressing to residents, said Brendan Williams, president and CEO of the New Hampshire Health Care Association.
“It’s discomforting to the residents to have strangers by the bedside,” he said.
Kindopp agreed, adding the high turnover with contractors is often at odds with delivering quality care.
“When staff get to know residents on an individual basis in ways that they can predict their needs and meet them … that is what providing good care can look like,” she said.
One of the most challenging pieces of the federal mandate is the requirement of having a registered nurse (RN) in the building at all times, administrators say. Prior to these changes, RNs were only required to be on site for eight hours a day.
“We used to have an RN in the building at all times, but in the past few years, we have struggled to hire RN’s for the overnight shift in particular,” said Kindopp, who noted that Maplewood does have an RN on-call 24/7.
In New Hampshire, the vacancy rates for RN positions are 17 percent, according to Williams, well above the national rate of 10 percent.
“Right now it’s a marketplace of desperation and scarcity,” Williams said.
Kindopp is still combing over the new federal rules to determine whether Maplewood will be considered a rural facility, and thus have longer to adopt the requirements. As always, she is looking to hire, while also maintaining her focus on providing the best possible care to the people who call Maplewood home.
“We want to hire more high quality staff, but in the absence of the availability of these individuals, we focus on meeting the needs of our current residents and choose to admit — or not admit — based on their needs and our ability to meet those needs with our current staff,” she said.
Williams — who expects the rules to be challenged in court — said that the longer timeline for rural facilities does nothing to address the issue when staff just aren’t available.
“There’s no magic wand that’s going to suddenly make [this requirement] feasible for nursing homes,” he said.




 Hospitals sue state over NH’s Medicaid tax
Hospitals sue state over NH’s Medicaid tax Federal officials to review Bow parents’ free speech lawsuit regarding transgender athletes
Federal officials to review Bow parents’ free speech lawsuit regarding transgender athletes  Flooding from collapsed beaver dam shuts portion of Elm Street in Concord
Flooding from collapsed beaver dam shuts portion of Elm Street in Concord Bassett to retire from New Hampshire Supreme Court
Bassett to retire from New Hampshire Supreme Court
